Insights from ASCO 2023: #2 – Patient Centricity
Curation and foreword by Kshipra Desai PhD, CMPP, Scientific & Medical Services Director – Nucleus Global, an Inizio Company
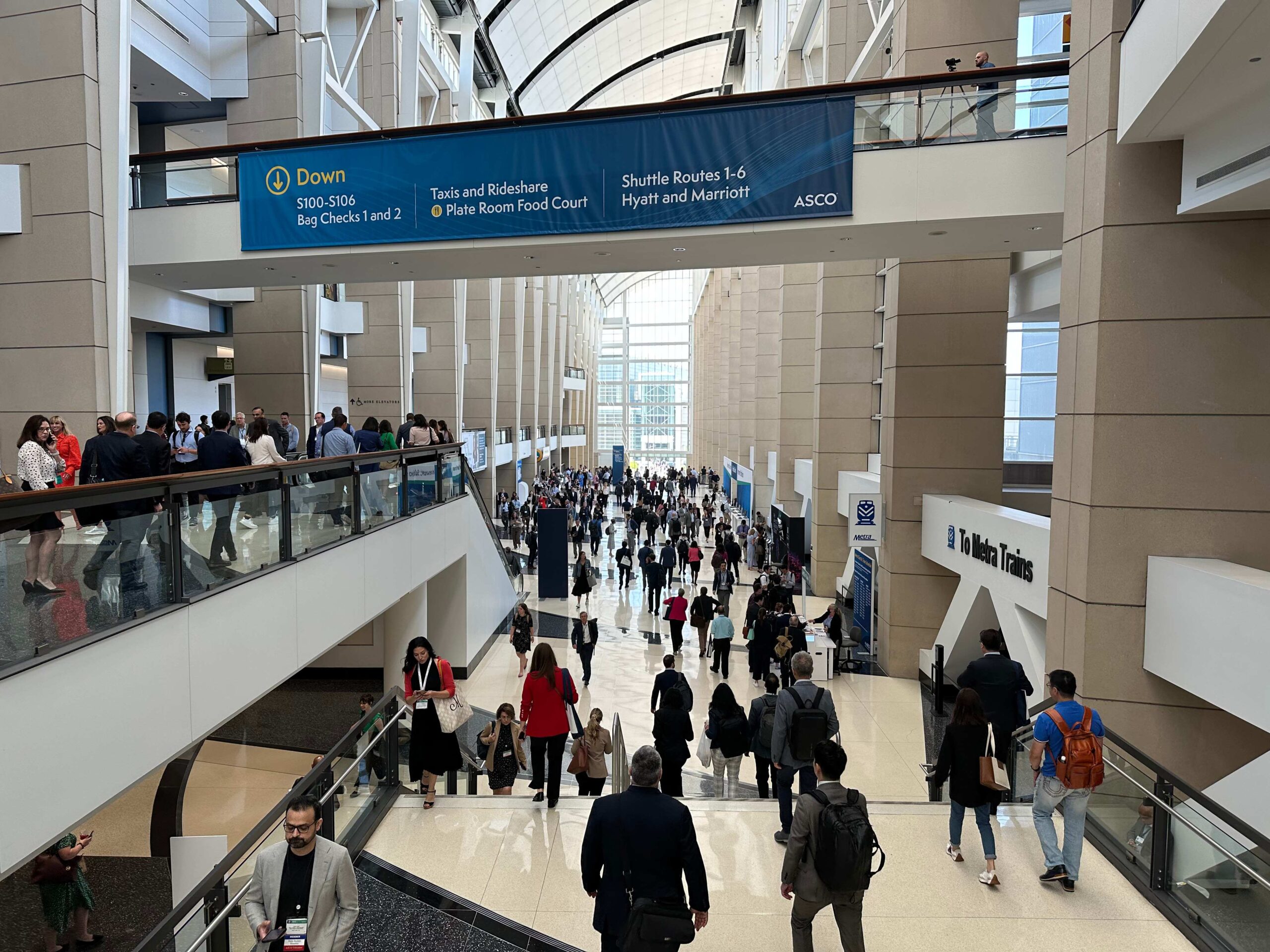
ASCO 2023 was back with a bang! With attendees having weathered the past three years of the pandemic, the atmosphere at the McCormick Convention Center was palpable as the 2023 meeting got underway. The meeting was one of the biggest in ASCO’s history, with 43,000 attendees, 36,000 of whom were there in person in Chicago. The theme of this year’s meeting was “Partnering with Patients: The Cornerstone of Clinical Care and Research.”
Our blog series (blog 1 available here) highlights some of the presentations less likely to be covered by conventional post-ASCO clinical wrap-up summaries.
In the second part of our series, we share insights from across the Inizio expert network into the evolution of cancer care and look at how it has evolved into a narrative of hope and holistic healing. No longer a relentless battle, it’s about living with cancer, enabled by advances in prevention, diagnosis, and treatment. The blog simultaneously explores the persistence of disparities in cancer care stemming from underrepresentation in clinical trials and unequal access to resources and how bridging these gaps demands open dialogue.
Addressing social determinants of health, particularly financial barriers, is crucial. Financial navigation programs offer relief, but their reach must expand to combat the financial toxicity of treatment. Simultaneously, integrating digital health tools and patient-reported outcomes (PROs) into care promises improvements, provided equitable access is ensured. As we navigate this transforming landscape, our goal is clear: cancer care that is accessible, equitable, and hopeful for all – read on as we explore how to make this a reality.
Partnering with Patients – Making it Real
Authors: Erinn Gideons PhD, Senior Medical Writer & Allison Lytle PhD, Lead Medical Writer – Nucleus Global
Faculty: Eric Winer, MD (Yale Cancer Centre), Michael Milken, Lynn Chehab, MD, MPH
Instilling hope in patients is critical for their overall wellbeing and willingness to be an active participant in their cancer treatment. Even 15 years ago, there was not as strong a sense of hope for patients diagnosed with cancer but due to the advancements in preventative care, diagnostic tools, and treatment, this has changed. A common metaphor has been “cancer is a battle”, but for patients with cancer, fighting feels like a struggle and does not engender optimism. Living life while having cancer is more encouraging than a never-ending battle. Patients need a provider that can motivate them and keep them hopeful in order to continue their treatments. Doctors should be supportive of their patients and remember to encourage not only their treatment successes, but their life outside of the disease. The job of the physician is to get people out of the clinic, not keep them in it.
Disparity in cancer treatment is a major concern, not only for patients but also for physicians. Disparity starts at the clinical trial level, as the populations in most clinical trials do not resemble the general population, due to the overrepresentation of White people in clinical trials. Additionally, not all patients have the same access to care due to lack of resources, insurance, or knowledge, among other issues. The interaction between the patient and doctor can also present a barrier to equity in treatment, as one bad interaction can make the patient doubt not just that doctor, but all doctors at that institution. Many patients are scared to bring up alternative treatments with their physician or even request a second opinion. Physicians are encouraged to support their patients if the addition of the alternative treatments won’t hurt them. Second opinions can also be beneficial to bring in a new perspective, as the amount of treatment options grow due to accelerating research in oncology.
Key insights:
- Doctors can be instrumental in instilling hope and motivation in their patients with cancer
- Increasing equity in cancer treatment can start with better recruitment of under-represented populations for clinical trials

Improving Cancer Outcomes by Addressing Social Determinants of Health
Erinn Gideons PhD, Senior Medical Writer & Allison Lytle PhD, Lead Medical Writer – Nucleus Global
Faculty: Ruth C. Carlos, MD, MS (University of Michigan), Reginald Tucker-Seeley, ScD (Zero – The End of Prostate Cancer); Chanita Hughes Halbert, PhD (University of Southern California)
Social determinants of health (SDOH), as defined by the World Health Organization, encompass the conditions that people are born, grow, live, work and age in, and the drivers of these conditions. It is well established that deprivations in these conditions produce poor health outcomes and the differences in the distribution of these deprivations produce community-wide health care-related disparities. It has been shown that people living in areas of greater deprivation of SDOH have lower rates of cancer screening and increased risk of dying. In recent years, research has been conducted at all levels to assess how to integrate this pre-existing knowledge into clinical spaces to address these social needs on both an individual and community level.
One of the greatest drivers to SDOH deprivations is lack of financial resources. The financial toxicity of increased costs of cancer treatment is associated with extreme distress, medication nonadherence, delayed visits and testing and postponed purchasing of items not related to treatment.
Financial navigation programs have been successful in assisting patients access resources that can help with all the costs associated with cancer treatment. However, more work is needed to assist the growing number of patients in need, including implementing them at multiple levels, and ensuring they are systematic, specific, and sustained. Precision therapy demands precision reduction in adverse events, including financial toxicity.
Key insights
- For programs addressing social determinants of health to be successful, there needs to be buy-in from many levels (providers, patients, and healthcare executives)
- Financial toxicity is an adverse event of cancer care and health equity issue that needs to be addressed with interventions at multiple levels
- Additional research is needed to develop tools to address social risk factors
Patient-Reported Outcomes, Digital Health, and the Quest to Improve Health Equity
Author: Matt Brierley, Director, Client Engagement – Ashfield MedComms
Faculty: Claire Frances Snyder, PhD (Johns Hopkins University School of Medicine); Gita Thanarajasingam, MD (Mayo Clinic); Debra A. Patt, MD, PhD, MBA, FASCO (Texas Oncology)
The session highlighted the challenges of expanded digital health in oncology, the value of direct patient engagement using PROs, examples of PRO implementation, and the evidence of improving cancer care delivery equity with the help of PROs. The use of ePRO was accelerated by the COVID pandemic.
PRO implementation can potentially lead to improved symptoms, functioning, quality of life, and satisfaction with care. Benefits and efficiency have also been shown, such as less emergency department use. And some studies have even shown that routine PRO monitoring increases survival.
In addition, electronic PRO reporting was associated with lower cost, better quality, equal or faster time of completion, less administrative burden, as well as being generally more preferred. However, these electronic systems run the risk of inadvertently excluding vulnerable populations with less ability to use or access technology.
Although a review reported that PRO interventions were generally feasible and acceptable in diverse and underrepresented patient populations, they did find some disparities for racial and ethnic minority patients, patients who speak Spanish (US focus of talk), patients with lower income, employment status, education, and health literacy, and older populations. Implementing ePRO into the clinic requires education, both for the staff and for the patients (regardless of clinical trial participation) and represents an opportunity for medical education specialists.
Implications
Collectively, the ASCO 2023 sessions highlighted the evolving landscape of oncology research and patient care, driven by advancements in AI, real-world data, patient engagement, and innovative technologies. As the field continues to evolve, the focus remains on improving outcomes, reducing disparities, and putting the patient’s voice at the forefront of decision-making.
Patient centricity was a notable recurring theme throughout the sessions. The value of physician-patient partnerships, the need for greater equity in treatment access, and the potential of digital health solutions, such as PROs, to improve cancer care delivery will all be pivotal in instilling hope, addressing social determinants of health, and enhancing patient engagement.

Jump to a slide with the slide dots.
Frequently Asked Questions About Building an Effective Scientific Communications Platform
Emerging biotech companies are at the forefront of innovation across the pharmaceutical industry. Leveraging cutting-edge science and inherent agility
Read moreAI’s Transformative Influence on Medical Communications
Discover AI's impact on medical communications, aiding HCPs with complex data and patient care. Download our eBook to learn more.
Read moreBeginning at the End: An Effective Strategy for Commercial Success
Employing an effective strategy For emerging biotech companies at the beginning of their product development journey,...
Read moreInizio Medical Issues Urgent Call to Action for AI Adoption in HCA Statement
A newly published AI roadmap, co-authored by the Healthcare Communications Association (HCA) and Inizio Medical’s...
Read more
