Insights from ASCO 2023: #1 – Drug Development and Clinical Trial Design
Curation and foreword by Kshipra Desai PhD, CMPP, Scientific & Medical Services Director – Nucleus Global, an Inizio Company
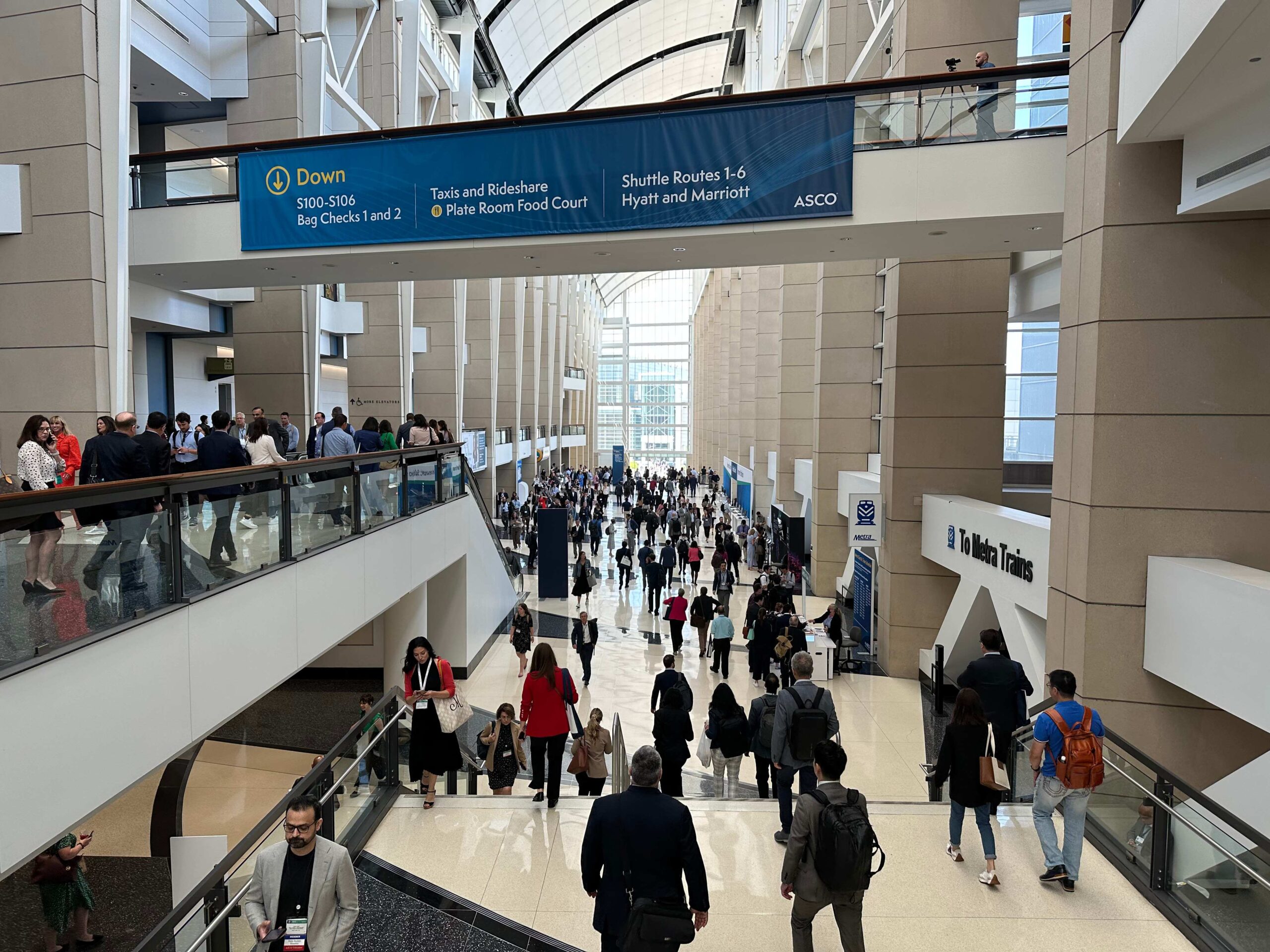
ASCO 2023 was back with a bang! With attendees having weathered the past three years of the pandemic, the atmosphere at the McCormick Convention Center was palpable as the 2023 meeting got underway. The meeting was one of the biggest in ASCO’s history, with 43,000 attendees, 36,000 of whom were there in person in Chicago. The theme of this year’s meeting was “Partnering with Patients: The Cornerstone of Clinical Care and Research.”
Our blog series highlights some of the presentations less likely to be covered by conventional post-ASCO clinical wrap-up summaries.
In the first blog of this series (blog 2 available here), we journey through the insights shared by trailblazing minds, each contributing to a mosaic of progress and change.
This blog delves into a series of thought-provoking discussions led by prominent experts in the field, shedding light on the transformative potential of artificial intelligence, real-world data, patient-centric clinical trial design, and accelerated approvals in oncology. As we navigate this complex terrain, it becomes evident that the convergence of these elements holds the key to more effective treatments, better patient outcomes, and equitable access to life-saving therapies.
In an era where the patient’s voice grows stronger and medical advancements are poised to make a profound impact, expert authors from across Inizio uncover the dynamic forces shaping the future of drug development and clinical trial design. Welcome to a world where science, compassion, and innovation intersect to pave the way for a brighter future for patients.
Artificial Intelligence for Drug Development: Fad or Future?
Author: Matt Brierley, Director, Client Engagement – Ashfield MedComms
Faculty: Arsela Prelaj, MD (Fondazione IRCCS Istituto Nazionale Tumori), Dean Ho, PhD, BS, MS (National University of Singapore), Alexander T. Pearson, MD, PhD (University of Chicago)
I3LUNG is a European project founded by the European Commission which involves 16 partners. The main goal is to develop a data storage platform housing real-world data and multiomics data in non-small cell lung cancer. The aim is to build AI-powered decision-making tool to predict immunotherapy efficacy and outcomes. The first cohort of 2,000 patients is being enrolled retrospectively (to date 1,576 patients). The first output is expected later this year. In parallel, translational data for the last 10 years from various centers is being analyzed and includes images as well as all the multiomics and lab test data. The key output will be an algorithm that can help guide decision making for those hard-to-treat cases in NSCLC.
Dr Ho discussed the role of AI I drug development and dose optimization and interestingly, how do we use AI to dynamically modulate dosing, for example, as the patient undergoes treatment to sustain optimization. He pointed out that we largely think about taking big data sets from diverse populations, training an algorithm, and then using that algorithm to treat the next patient. However, he wanted to depart from this model and instead talk about digital avatars, and indeed not use any pre-existing data to treat the next patient. The concept is to prospectively calibrate that individual patient by measuring different parameters, for example how they respond to different doses all within allowable ranges and with corresponding biomarkers. This way the physician is only using a patient’s own data to only modulate their care throughout their treatment. Dr Ho’s team have shown that in some cases at the right time reducing doses can improve efficacy. This approach can also identify when a treatment is not going to work, and so a drug is required. This is an interesting approach to personalizing patient care and runs alongside more traditional population-based clinical trials. The approach requires continuous and ongoing interaction between the healthcare team, AI and the patient. It will be interesting to see how this research moves forward and how comfortable both prescribers and patients will be in real world settings if this approach becomes available in the clinic.
Dr Pearson spoke about applications of AI for pathology image-based detection of clinically actionable genetic alterations. His two learning objectives were to describe:
- Relevant techniques for developing artificial intelligence-based biomarkers for predicting molecular states and provide examples of biomarkers in advanced clinical development worldwide
- Sources of bias for AI biomarkers and the best practices to counteract deploying biased models into practice
He described a method of deep learning that can extract additional information from pathology images down the pixel level. Spatial information at this level can undergo mathematical modelling and generate extra layers of data. Dr Pearson highlighted that AI is already being used in the identification of cancer cells and in parallel to identifying molecular targets in a patient. The goal is to make an AI platform in pathology that is bias free (applicable to each individual patient) as well as generalizable (applicable to all patients). This is clearly an active area for AI research and development.
Overall, the speakers championed the introduction of AI into healthcare, highlighting its positive impact from drug discovery, through to diagnosis and indeed treatment decisions. All the speakers however, underlined the need for close physician oversight and independence of thought when the multidisciplinary care team are deciding the best course for an individual patient.

Patient-centric Clinical Trial Design in Genitourinary Cancers: Meaningful Endpoints, Assessments, and Outcome Measures
Author: Scott Battle PhD, Lead Medical Writer – Nucleus Global
Faculty: Benjamin Miron, MD (Fox Chase Cancer Center), Dena Battle, BS (KCCure), Elizabeth Marie Wulff-Burchfield, MD (University of Kansas Medical Center)
Real-world data of patient health status and/or delivery of health care and can be collected from a variety of sources. Real-world data are valuable resources, however, missing data, especially in the form of exclusion of a certain class of patients, can introduce bias. Real-world data can support clinical trial design, including providing power calculations or efficacy targets when historical trial data no longer reflect real-world standard of care, control arm design based on contemporary patterns of care, and site selection to ensure the target patient population can be recruited. Further, real-world data can be used to improve trial eligibility criteria, reduce restrictions and improve outcomes, and eligibility criteria that are not necessary may contribute to perpetuating disparities in access to clinical trials.
Real-world data can be used to assess treatment patterns, but they may not capture patient priorities and understanding. Evidence-based information can be used to better design clinical trials that best answer questions important to patients instead of following established clinical trial models, giving patients a greater voice in the process.
The value of any cancer treatment goes beyond the traditional efficacy and safety measurements. There is often inconsistency between how physicians and patients assess treatment toxicity, with the physician more likely to underestimate the severity, and this discordancy is associated with increased patient distress and worse quality of life. Patient-reported outcomes (PROs) are critical to capturing the patient voice in clinical trials and should be used in triangulation with efficacy and physician-reported toxicity assessments to evaluate the value of treatment. However, establishing which PRO measurement tool to use can be difficult (eg, general vs disease-specific tool and ensuring multicultural utility and validity with evolving patient populations and standards of care). Therefore, trends in PRO measurement over time rather than absolute numerical scores should be evaluated, such as if treatment is associated with a quality-of-life improvement or a delay in deterioration over the course of the study. Overall, real-world data are a powerful resource to help guide clinical trial design and potentially improve patient outreach, engagement, and voice.
The Future of Equitable Access to Clinical Trials
Authors: Matt Brierley, Director, Client Engagement – Ashfield MedComms & Michael Demars PhD, Associate Scientific Director – Nucleus Global
Faculty: Steven Gore (National Cancer Institute), Ana Acuna-Villaorduna, MD (Montefiore Medical Center/Albert Einstein College of Medicine), Lola A. Fashoyin-Aje, MD, MPH (U.S. Food and Drug Administration))
The clinical trial process has been improved over recent decades leading to drastic increases in the number of cancer drugs approved by the FDA, and increased response rates in early-phase clinical trials. However, barriers to access exist at the patient, provider, study, and institution level despite continual improvements to the process. These barriers result in disparities between study and real-world patient populations where minority groups (race/ethnicity, sex, age, and geography) are often underrepresented in clinical trials, especially in early phase trials. Such disparities can impact the generalizability of trial results, efficiency in delivery of care, understanding of drug pharmacodynamics and pharmacokinetics in underrepresented populations, and early access to potentially efficacious investigational treatments in underrepresented groups. Therefore, it is essential that trial designs and recruitment processes result in study populations that represent the intended target population of the medical products submitted for regulatory review.
Key questions were raised.
- How do we manage to recruit patients into trials from geographical, socio diverse populations into trials?
- Do trials run from often city-based centers in relatively affluent areas exclude patients in rural and socially deprived areas
Organizations (including the FDA and Experimental Therapeutics Clinical Trials Network) have programs in place to drive inclusion of these underserved patient populations and indeed have provided guidance on diversity action plans. Regulatory frameworks are changing to ensure all patients are adequately represented in trials. It will not be surprising to see this mirrored in other medical settings such as for publications presenting clinical trial data. Although patient characteristics are typically included there may be a call to provide more information as to the patient population recruited and studied and to demonstrate that this truly represents the real-world patients treated in that therapy area. Ultimately, the aim of these programs and frameworks is to better ensure that trial populations look more like the real-world populations that treatments are intended for.
Accelerated Approvals in Oncology: Balancing Access with Evidence
Authors: Bryan Hodson PhD, Associate Medical Writer & Allison Lytle PhD, Lead Medical Writer – Nucleus Global
Faculty: Walid Gellad (University of Pittsburgh), Romeo Angelo M. De Claro, MD (U.S. Food and Drug Administration), Andrew James Schorr (PatientPower.info)
The FDA’s Accelerated Approvals process was initiated in 1992 to combat the HIV/AIDS crisis via conditional approvals for novel agents. These agents needed to treat a serious condition, demonstrate meaningful clinical advantages over current therapies, and importantly they required confirmatory trials post approval. There has been an exponential increase in the number of approvals each decade since the start of the program (18, 37, and 123 in the first, second, and third decades respectively) with a more recent shift toward oncology (62% overall, and 76% in the last 5 years). However, challenges emerged with the withdrawal of agents (12.4%) after confirmatory trials were negative.
These withdrawn agents had a longer overall time in the marketplace before the confirmatory trial results led to withdrawal. The average time to withdrawal was 4.1 years overall: 3.1 years for agents with verified clinical benefits vs 7.3 years for those withdrawn which had no ongoing confirmatory trials at approval. Medicare and Medicaid paid $18 billion from 2018 and 2021 for agents with delayed confirmation, including approximately $700 million for one single agent (hydroxyprogesterone caproate), which was later withdrawn when the confirmatory trial failed. On December 29, 2022, FDORA (the Food and Drug Omnibus Reform Act) was passed that made changes to the Accelerated Approvals process; it formed an Accelerated Approvals council for evaluation on a case-by-case basis, updated procedures for both withdrawal and reporting of post-marketing studies, and added the requirement for confirmatory trials to be underway before an approval is granted.
While these legislative changes were designed to reduce unnecessary costs for medical payers, FDORA did not address some of the challenges patients endure because of the regulatory process, which patients view as sometimes needlessly burdensome. The current regulatory processes still cause challenges for patients who experience delayed access to novel agents, potential trouble reaching trial sites, and a perceived lack of communication about the existence of trials from healthcare providers.
One patient stated “I wouldn’t want to go to my grave, knowing that there’s a drug out there that might benefit me, but the FDA says I can’t try it. I want to try it, even if I have to take the risk that we don’t know all the side effects behind it.”
This balance between confirmed efficacy, a need for cost-effective therapies, and the patients’ desire for access to novel, potentially life-saving therapies is difficult. FDORA has made progress in addressing challenges in the regulatory approvals process for such therapies, allowing reduction of withdrawals, reduced time to confirmation, and earlier access to novel agents for serious conditions for patients.
Key Insights:
- FDORA added a requirement that confirmatory trials be ongoing to qualify for Accelerated Approvals in an attempt to reduce delays in confirmatory approvals and reduce the rate of withdrawal.
- However, patients facing rare and life-threatening diseases are more willing to take risks and favor speedier regulatory approvals.
Integrating Liquid Biopsies into Patient Care and Clinical Trial Design
Author: Asu Erden PhD, Scientific Director – Nucleus Global
Faculty: Tyler Paul Johnson, MD (Stanford University Hospital) who was the moderator, and three panelists, Luis A. Diaz, MD (Memorial Sloan Kettering Cancer Center), Lillian L. Siu, MD, FASCO (Princess Margaret Cancer Centre), and Peter Gibbs, MD, FRACP, MBBS (Royal Melbourne Hospital).
This panel of experts discussed the clinical applications of circulating tumor DNA (ctDNA) through hypothetical cases studies. Panelists agreed that increased patient awareness of liquid biopsy as a non-invasive testing method is accelerating its integration into routine cancer care. However, healthcare teams should remain cautious as to insights provided by positive and negative ctDNA results. While the prognostic value of a positive ctDNA results has been established, the predictive value of ctDNA results remains poorly studied. The latter area of research is ripe for dedicated randomized, clinical trials, especially in the metastatic setting. It is also important to remember that intra-patient changes in ctDNA occur based on surgery, treatment, and tumor location. Differences also exist in the insights provided by tumor-informed ctDNA assays—which are typically used in earlier stage disease, are more sensitive, lead to fewer false positives, but have longer turnaround time—and tumor-agnostic ctDNA assays—which are typically used in advanced and metastatic stage, are less specific and sensitive, but have faster turnaround times. These assays can also vary in the lead-time between ctDNA positivity and clinical or radiographic progression. As such, most liquid biopsy tests ordered are primarily informative and add to the research dataset. Additional investigational efforts are needed to understand the relationship between the natural history and biology of specific tumors (eg, shedders vs non-shedders, anatomic barriers to ctDNA, impact of low tumor burden, lead-time) and associated ctDNA results.
Overall, the session’s take-home message focused on the evolving role of ctDNA in cancer care: ctDNA is fast becoming an integral component of clinical care and today’s research on its integration will establish tomorrow’s standard of care.
Implications
From the transformative potential of artificial intelligence to the power of real-world data in shaping clinical trial design, ASCO highlighted the rapid nature of change in the life science landscape.
AI is unquestionably revolutionizing drug development, not only by harnessing vast data sets but also by dynamically adapting treatments for individual patients. Real-world data is simultaneously emerging as a powerful resource, helping design more inclusive and meaningful clinical trials as patient voices grow stronger, influencing trial endpoints and measurements, ultimately leading to better outcomes.
Together, we are paving the way for more effective treatments, improved patient outcomes, and equitable access to life-saving therapies. The road ahead may be challenging, but with a shared commitment to progress, we can look forward to a future where science, compassion, and innovation intersect to create a world that reimagines the possibilities in drug discovery and clinical trial design.

Jump to a slide with the slide dots.
Frequently Asked Questions About Building an Effective Scientific Communications Platform
Emerging biotech companies are at the forefront of innovation across the pharmaceutical industry. Leveraging cutting-edge science and inherent agility
Read moreAdapting patient solutions in a changing biotech landscape
Nareda Mills, Global President of Patient Solutions at Inizio Engage, highlights the need to adapt patient solutions and explains how biotech chan..
Read moreAI’s Transformative Influence on Medical Communications
Discover AI's impact on medical communications, aiding HCPs with complex data and patient care. Download our eBook to learn more.
Read moreInizio Medical Issues Urgent Call to Action for AI Adoption in HCA Statement
A newly published AI roadmap, co-authored by the Healthcare Communications Association (HCA) and Inizio Medical’s...
Read more
